What is a Bronchoscopy?
What is a Bronchoscopy?
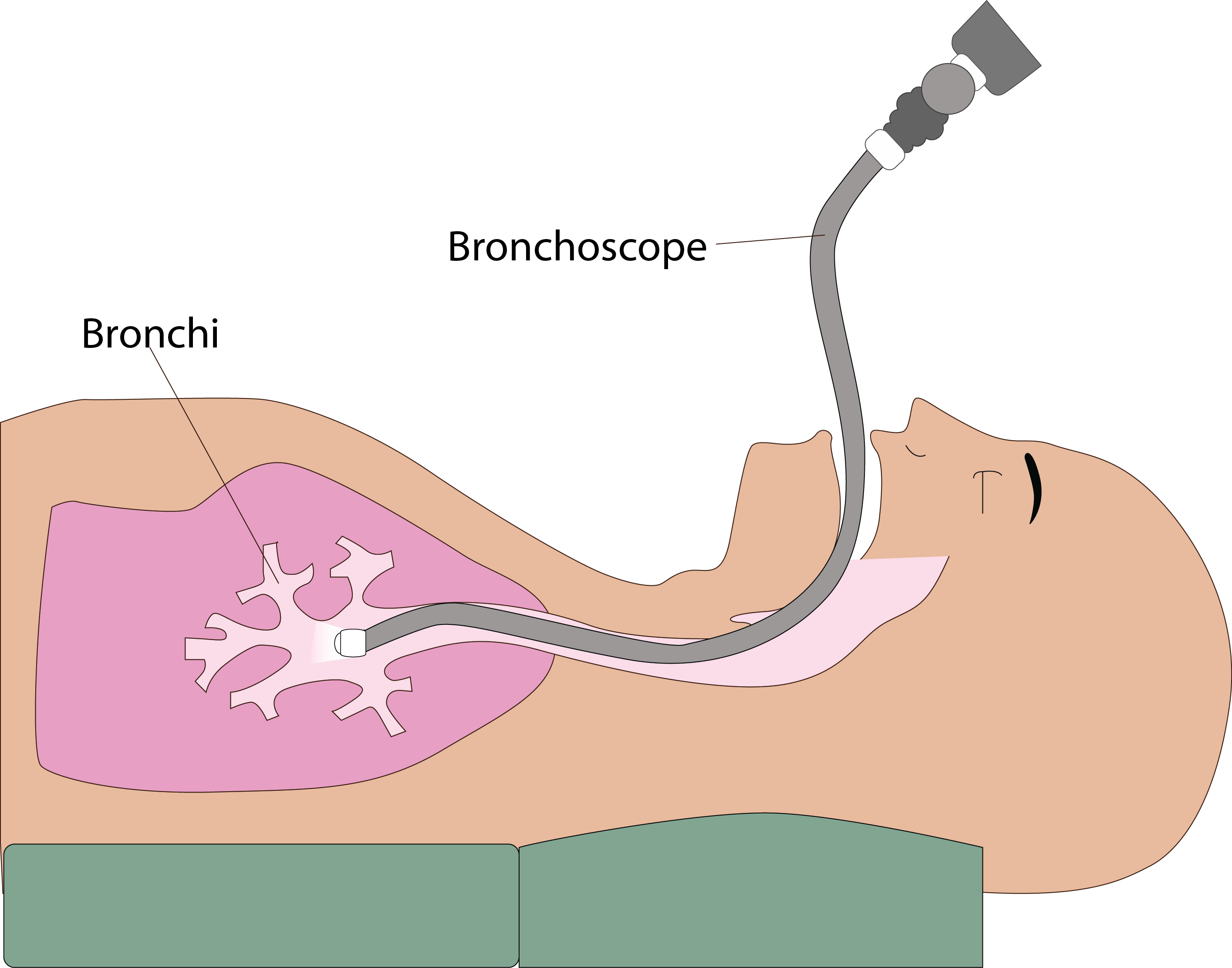
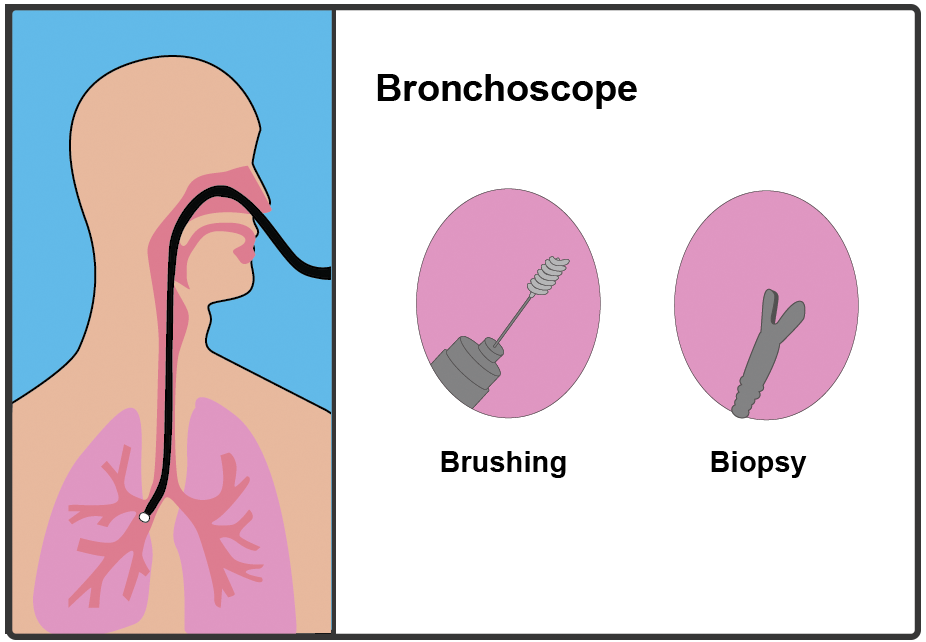
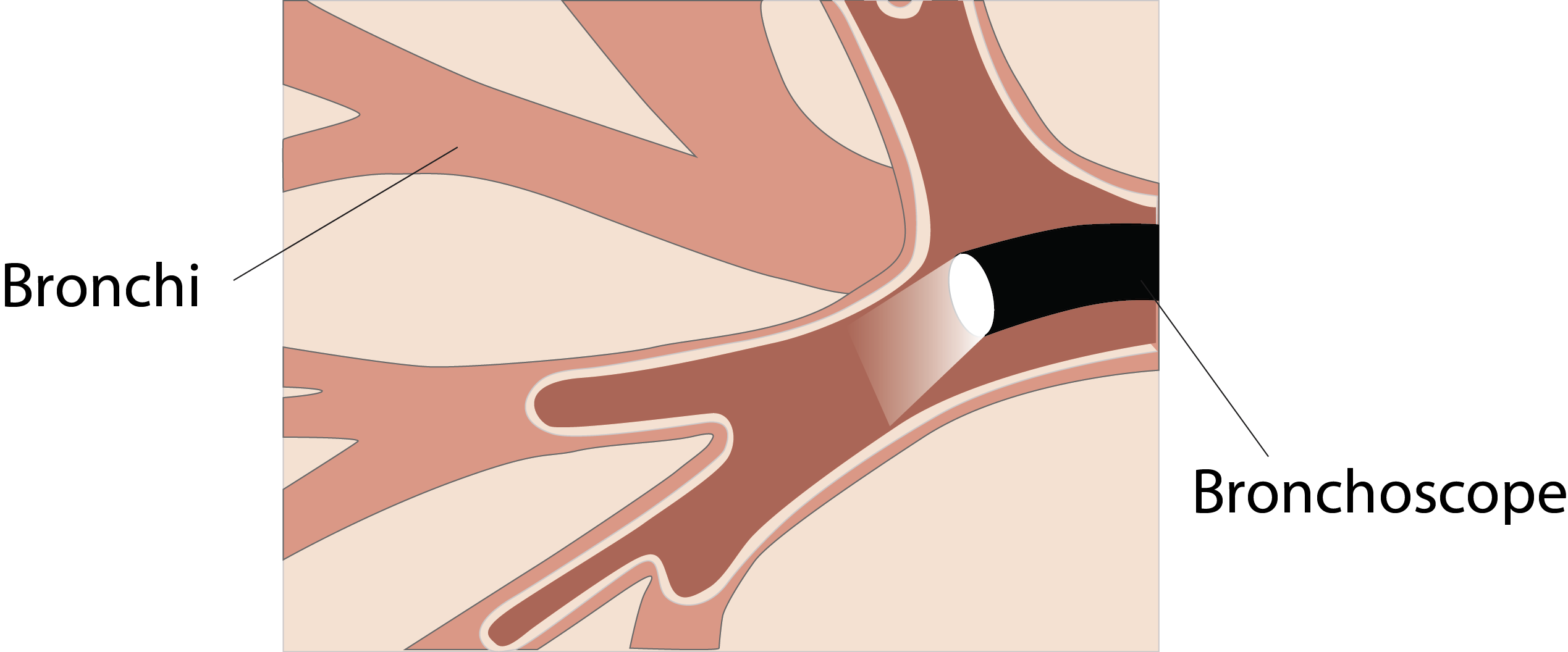
A bronchoscopy is a camera test to look at airways ("breathing tubes") in your lung. A thin, long flexible tube with a light and camera at the end called a bronchoscope is used to look at your airways. If necessary your doctor can collect samples (such as fluid, mucus and biopsies) with the bronchoscope and send them to the laboratory for further examination.
Why do I need a Bronchoscopy?
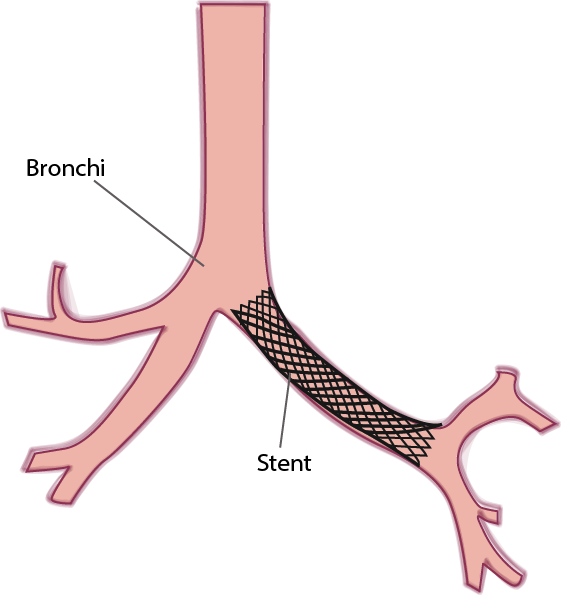
Common reasons for having a bronchoscopy include an abnormal shadow on an X-ray, coughing up blood, recurrent chest infections, unexplained breathlessness, unusual chest infection or persistent cough. A bronchoscopy can also be performed to remove a foreign body or mass from the airway or to insert a tube (stent) to open up an area of lung that is collapsed.
Before the Bronchoscopy
You should not eat or drink anything (fast) for 4 hours before your bronchoscopy. In some cases your medical team may instruct you to fast for longer.
Please tell the doctor or nurse if you have any allergies.
Please tell the doctor or nurse if you are on any medications to thin your blood or medications to stop your blood from clotting such as Warfarin, Dabigatran (Pradaxa), Apixaban (Eliquis), Rivaroxaban (Xarelto), Clopidogrel (Plavix) or Aspirin.
Procedure
You will be given medication (sedation) to make you sleepy and unaware of the procedure but you will not be fully unconscious as occurs with a general anaesthetic.
You will be asked to sign a consent form.
A small plastic tube (line) will be put in your hand or arm. This will allow the doctors to give you medication (sedation) to make you sleepy during your test.
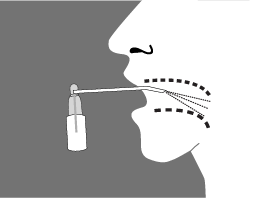
The back of your throat will be sprayed with a local anaesthetic spray to make it numb. It may taste a bit unpleasant. A plastic mouth piece will be put in your mouth. You will be given some medication to make you sleepy through the plastic line in your hand.
Occasionally a nasal spray will be performed also or instead to allow looking at the nose at the same time.
When you are sedated, the bronchoscope will be passed through your mouth or nose. When it is just above your voice box, local anaesthetic will be injected down the bronchoscope. The camera will then be passed into the main airway (trachea) and onwards to the smaller branches (bronchi). As needed additional local anaesthetic will be injected into these airways.
The doctors will look carefully at your airways.
Depending on why you are having a bronchoscopy performed the doctors may perform additional procedures. These include:
1. Washings - sometimes salty water (saline) is injected into your airways and sucked back out. This salty water can then be sent to the laboratory for analysis.
2. Biopsy - A small needle/ forceps may be used to take a sample of lung tissue or a mass if one is seen.
3. Brushings - a soft brush is sometimes used to get a sample of cells from the airway to send to the laboratory for analysis.
After the Bronchoscopy
You will be observed for 1-2 hours after the bronchoscopy while the drowsiness is wearing off.
You should not eat or drink for 1-2 hours after the test as you will still be a little sleepy and your throat will still be a bit numb.
You should not drive for 24 hours after the test and so you will need to ask somebody to collect you after the bronchoscopy.
What are the risks?
Bronchoscopy is a very safe procedure and the majority are performed without any problem.
Minor symptoms/ complications:
You may experience a sore throat, cough, fever or sweating for the first 12 hours after the bronchoscopy. These symptoms typically resolved without any treatment or by taking a low dose of paracetemol (2 tablets) on one occasion. Some patients may cough up a small amount of blood (less than a teaspoonful) after having a bronchoscopy and biopsy. You will still be drowsy after the procedure and should not drive for 24 hours after having a bronchoscopy.
More serious symptoms/complications:
Infection - some patients may develop a chest infection after a bronchoscopy. If you cough up dark phlegm, have an ongoing temperature or are feeling particularly chesty in the days following your bronchoscopy you should contact your GP who can advise you about the need for antibiotics.
Collapsed Lung (pneumothorax) - Occasionally some patients may get a Collapsed lung (pneumothorax)after bronchoscopy. This is unlikely to occur unless you are one of a smaller number of patients that need to have a special type of lung biopsy called a transbronchial lung biopsy performed. Your doctor will tell you beforehand if you need this test and you will have an x-ray afterwards to make sure than you do not have a collapsed lung. Some patients need a special tube (chest drain) to be put into the chest to help re-inflate the lung.
Medication - a small number of patients may be allergic to the medication given for sedation during bronchoscopy. Your doctor & nurse will ask you about medication allergies before this test.
Bleeding - on rare occasion patients may cough up larger amounts of blood and need to be admitted to hospital.
What are the Benefits of a Bronchoscopy?
Allows your medical team to inspect your airways thoroughly for infection, foreign bodies or potential tumours.
Allows your medical team to take samples from abnormal areas in the lung to diagnose your lung problem.
What symptoms should I look out for after the test?
You should contact your GP if you experience any of the following symptoms and are worried about them:
1. Persistent coughing up of blood.
2. Breathlessness.
3. Chest pain.
4. Persistent temperature and sweating lasting more than 48 hours.